Living with Fibromyalgia
It is important to remember that writing about any condition is always specific to each individual. My experience of having and living with an illness may be completely different from another person being diagnosed with the same condition. That is why it’s important not to treat us all in the same way and offer us the same advice.
I grew up in a house where my Mum had Fibromyalgia. I thought I understood it a little and knew what pain she was in. I had no idea until I started to suffer with it myself.
Fibromyalgia is often called the invisible illness and can take many years to diagnose. It is an umbrella term for many different symptoms grouped together, so it can often get overlooked or misdiagnosed.
What is it?
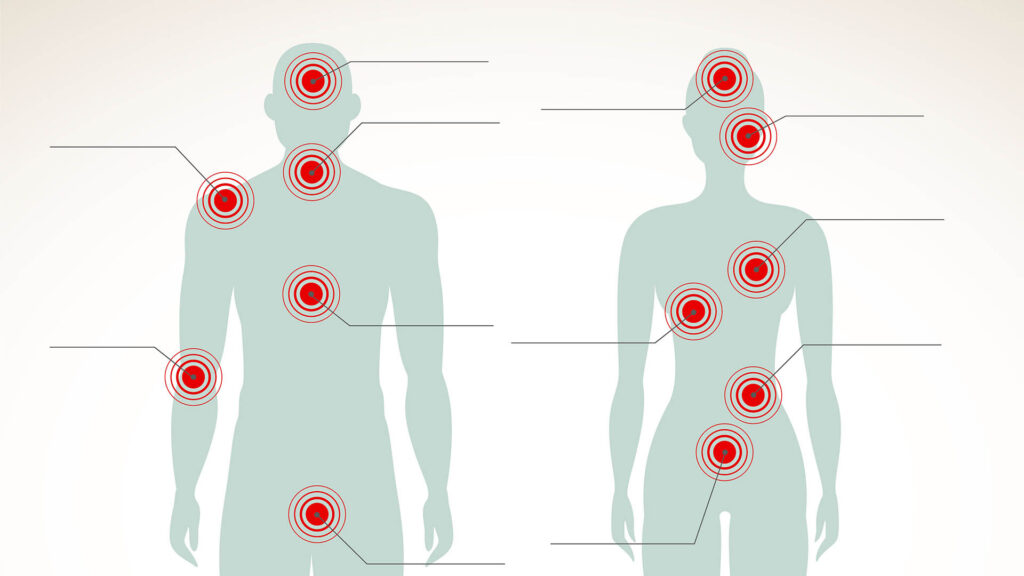
Fibromyalgia is a long-term chronic condition that can cause widespread pain all over the body. A medical professional can try to diagnose fibromyalgia by pressing on 18 points located throughout the body to identify any tenderness or pain. As not all people react the same way to this test, years can be spent trying different medications to stop additional symptoms from occurring.
It took me over 10 years to get diagnosed. Over the years my symptoms have intensified and have covered the following:
- Memory issues
- Confusion and Brain Fog
- Chronic Pain
- Migraines
- IBS
- Restless Leg Syndrome
- Fatigue
- Vertigo
- Excessive temperature fluctuations
- Extreme itching or Eczema
- Depression and Anxiety
- Suffering from constant urine infections or feeling you have them
- Vision issues
Because of the array of symptoms, I was sent to different specialists over the years who dealt with each symptom separately. This resulted in more tests, more time at the hospital and lots of medications. There were times I felt like a zombie because of the number of medications I was on.
It is the impact it has had on my life rather than dealing with each symptom that’s the most difficult part for me to deal with. When my symptoms were at their worst, I started to feel very down and depressed. The impact on your mental health can be just as debilitating. I didn’t want to go out and I couldn’t spend time with my family and friends. Eventually, many of my friends disappeared as they were fed up with the constant cancellations and couldn’t empathise with my condition. Losing friends in conjunction with the illness made me feel very isolated, alone, and angry.
One of the biggest contributors to poor mental health is not just the condition itself but what happens after the diagnosis. There is an ‘off you go’ attitude I’ve experienced by many specialists. There is no cure for Fibromyalgia; you are just expected to deal with it by yourself.
There was a huge impact on my family and work when my Fibromyalgia got worse. I was having more time off work and stressing about that which made me even worse. I then got into a cycle of stressing about having time off work which made me absent for long periods of time. I have two young children and my wife had to look after them and me. There is no guidance or support for them either. My wife and I would get frustrated with each other due to the situation we were in. I couldn’t do certain things for myself or was in bed for days which can be very frustrating for your partner when you have a young family.
The biggest ongoing symptom for me is fatigue. There is a huge misunderstanding about fatigue and tiredness. Tiredness is when you have had a long day or little sleep and you need to go to bed. Fatigue means that no matter how much sleep you have, you never feel refreshed. You can sit down and not know how you will get up to have a shower, get out of a chair or brush your teeth. It’s like your body is made from lead. Some days, daily tasks such as making the bed, walking up the stairs or changing the bins can seem like a huge challenge.
Then comes the medication. I have been put on dozens of medications over the years, some are successful and others have awful side effects. I have spent more time off work trying to wean off medications than dealing with the condition itself.
Each day is a challenge with Fibromyalgia. One day you will feel fine and want to do more. The next day you can’t get out of bed. I can start the day feeling great and then feel awful in a matter of minutes.
The final factor of having Fibromyalgia is its interaction with other illnesses. I suffer from a neurological illness where I have a permanent migraine and vertigo. Having Fibromyalgia interacts with this and causes the pain to intensify. Other people I have spoken to have mentioned how Fibromyalgia makes other illnesses worse.
There are however positive sides to dealing with this illness. I have had huge support from my managers and colleagues in IT Services at the University over the years and without that, I would no longer be at work.
My family constantly support me and because my children have grown up with me having the illness, they know how to deal with it on a bad day.
I have had mental health support both outside and within the University which allows me to deal with this condition on a daily basis. It is a condition with no respite, so strong mental health is key to dealing with it. I was told that being diagnosed with a chronic illness can illicit the same mental health symptoms as a bereavement. We long for the life we once had, and it is fine to ask for help to cope with that.
If you do not work on your mental health, then dealing with this disease is impossible. I know people who have this disease who no longer go to work and spend most of their time in bed suffering from depression.
I would say that my relationship with this illness now is better than it has ever been. I still have my low days, but I know with the right support and attitude, I can deal with it.
Gary Hale
Senior IT Services Specialist
Today (12 May) is World Fibromyalgia Awareness Day. More information about the condition can be found here.
Any staff member with a physical or hidden disability is welcome to join the Staff Inclusivity Group, which advocates for equality in the workplace for colleagues with physical or invisible disabilities. The group is also a place to seek support from one another and challenge University policies and practices.
Equity, Diversity and Inclusion
Reflections, comments, discussion and opinion on EDI topics from Loughborough University staff and students
Join the discussion
7 Comments
Dawn M
I had no ‘real’ idea about this condition until I read this Gary. I’d heard of it, but didn’t know what it was. Thank you for sharing and being so honest about how it’s made you feel over time and the challenges that you have had to overcome.
Andy T
Thank you Gary for sharing such an insightful story about the condition of fibromyaldia and how you live with it, it is a very thought-provoking read.
Steph Bourgault
It is really interesting to read how fibromyalgia affects you, Gary. My daughter has it, combined with Coeliac Disease and Ehlers Danlos Syndrome and it is quite hard to understand how they interplay with each other. Interestingly, in addition to Fibromyalgia Awareness Day and Mental Health Awareness Week, it is also Coeliac Disease Awareness Week – I’m guessing it isn’t a coincidence! Thank you for sharing and broadening our understanding.
Clive Woodhouse
A very honest account which I’m sure will help lots of people. Thanks Gary!
Pali Bains
Thanks for sharing Gary, I could never have imagined that fibromyalgia could cause so many issues, your story has certainly raised my awareness of this condition. You’re a great colleague that I have always found to have a cheery smile and laughed at my jokes – so long may that strong, resilient attitude continue.
steve rothberg
Wow, I learned a lot from your blog, Gary. thanks for sharing, I’m sure it’s not easy to tell the world how you feel but such a good thing that you did it
Nada Nassuhy
My sister was misdiagnosed and I felt lost and helpless, she had the symptoms like muscle cramps and spasms, joint pain and trouble in sleeping but after living very tough days we figured out the right path with the help of medical platform called docspert health. We met the doctor on zoom meetings and he was very helpful and guided us, so she didn’t need to go anywhere or travel abroad.